MediSuite-Ai-Agent
Automates claims intake, extracts medical billing data, reduces denials, and speeds approval cycles.
Trusted by
Built on proven document-intelligence and LLM-assisted workflows used by leading payers and RCM firms; designed for auditable outputs and configurable governance controls. (Amazon Web Services, Inc.)
Success Story
Anthem automated 80% of its claims-processing workflow after deploying AWS Textract, reducing manual extraction (20 min per claim) and scaling to thousands of claims/day.
Integrates with
Problem
Claims processing requires manual extraction of clinical and billing data from unstructured attachments. This causes long processing times, high denial rates, and heavy manual appeals work — increasing days-in-receivables and staff costs. Payers and revenue-cycle teams need faster, auditable first-pass decisions and fewer avoidable denials. (Amazon Web Services, Inc.)
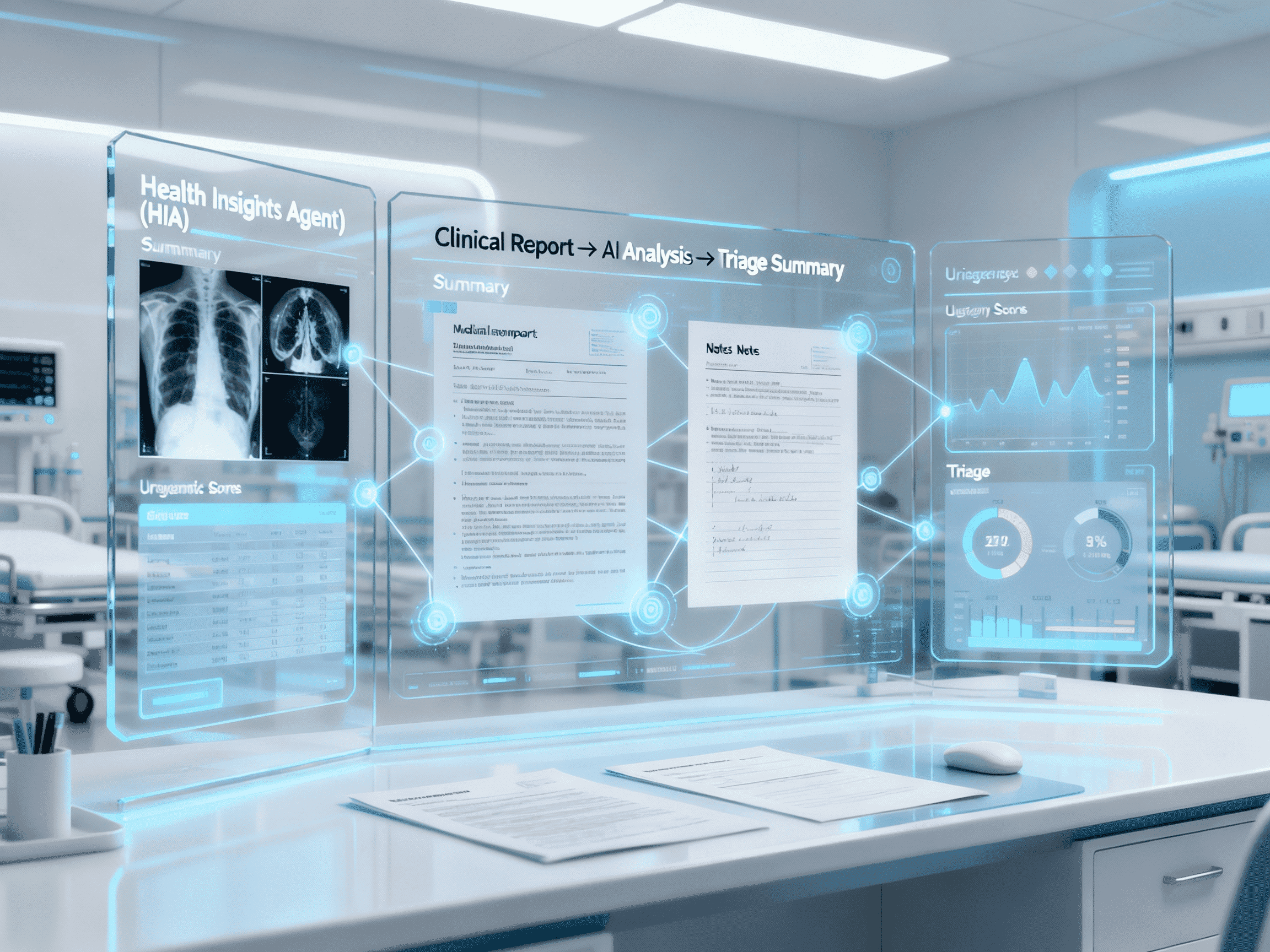
Solution
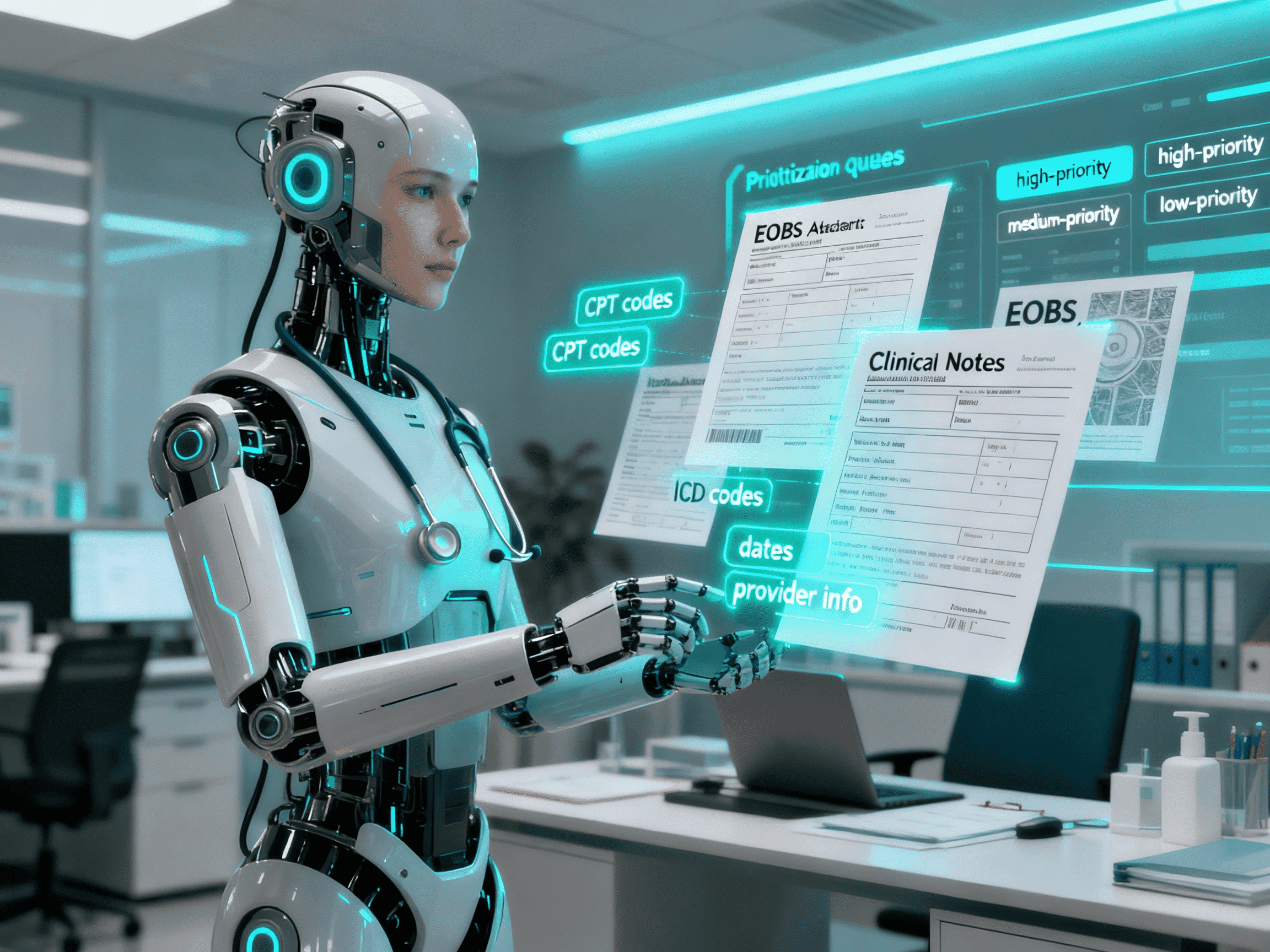
MediSuite ingests claims and attachments, runs OCR + clinical/billing extraction, validates entries against payer rules, assigns risk scores for denial, and produces recommended fixes and appeal text. It creates prioritized queues for adjudicators, enabling faster first-pass resolution and fewer manual corrections. (openai.com)
Result
Faster claim handling, fewer manual hours per claim, lower denial and appeal rates, and improved cash flow. Typical industry outcomes to aim for: 40–75% reduction in manual processing time, 30–50% lower turnaround for escalations, and measurable ROI within months (results vary by org).
Use Cases
MediSuite-Ai-Agent automates the repetitive, error-prone steps of health insurance claims handling. It ingests claims, scans attachments (clinical notes, EOBs, imaging reports), extracts structured data (CPT/ICD codes, dates of service, provider IDs), applies business rules for validation, and surfaces likely denials or missing information with recommended corrections and appeal language. The agent provides a prioritized worklist for adjudicators, creates standardized claim packets (CSV/JSON/PDF), and integrates with existing ticketing/storage systems to shorten cycle time and reduce appeals workload. Designed for payers, revenue-cycle managers, and hospital billing teams, MediSuite improves first-pass accuracy and reduces manual rework so human reviewers focus on clinical exceptions and value decisions. (Amazon Web Services, Inc.)
Integrations
Connect to your existing tools seamlessly
Technology Stack
Automation
Automation
Infrastructure
Implementation Timeline
Discovery & Sample Dataset Ingestion
1 weekCollect representative claims, attachments, and denial examples. Define KPIs and access controls.
OCR & Extraction Mapping Setup
1 weekConfigure OCR pipeline (Textract/Tesseract), create extraction templates, and map fields to downstream systems. (Amazon Web Services, Inc.)
Risk Rules & Checklist Configuration
1 weekBuild denial-risk rules, mapping to payer policies, and configure appeal suggestion templates.
Pilot Batch Review & Tuning
1-2 weeksRun pilot batches, measure extraction accuracy and false positives, tune models and thresholds. Use adjudicator feedback cycles. (Business Insider)
Integration with Storage, Notifications & Reporting
1 weekConnect to adjudication engines, EHR/FHIR endpoints where allowed, and dashboarding for ops and finance.
Handover, Training & Production Rollout
1 weekProvide docs, training sessions, run-rate monitoring, and post-go-live tuning support.
Support Included
Comprehensive documentation with step-by-step workflow setup, API configuration guides, integration instructions. Optional onboarding call and email support during the launch phase.