Lina-Egyptian-Medical-Chatbot
Automates claims intake, extracts medical data, reduces denials, and accelerates claim approvals for hospitals and insurers.
Trusted by
Built on proven IDP and LLM workflows used by leading payers and RCM firms; ensures auditable outputs and configurable governance.
Success Story
Anthem automated 80% of claims with AWS Textract, cutting manual extraction from 20 min per claim and scaling to thousands/day — example of comparable IDP, not this agent.
Integrates with
Problem
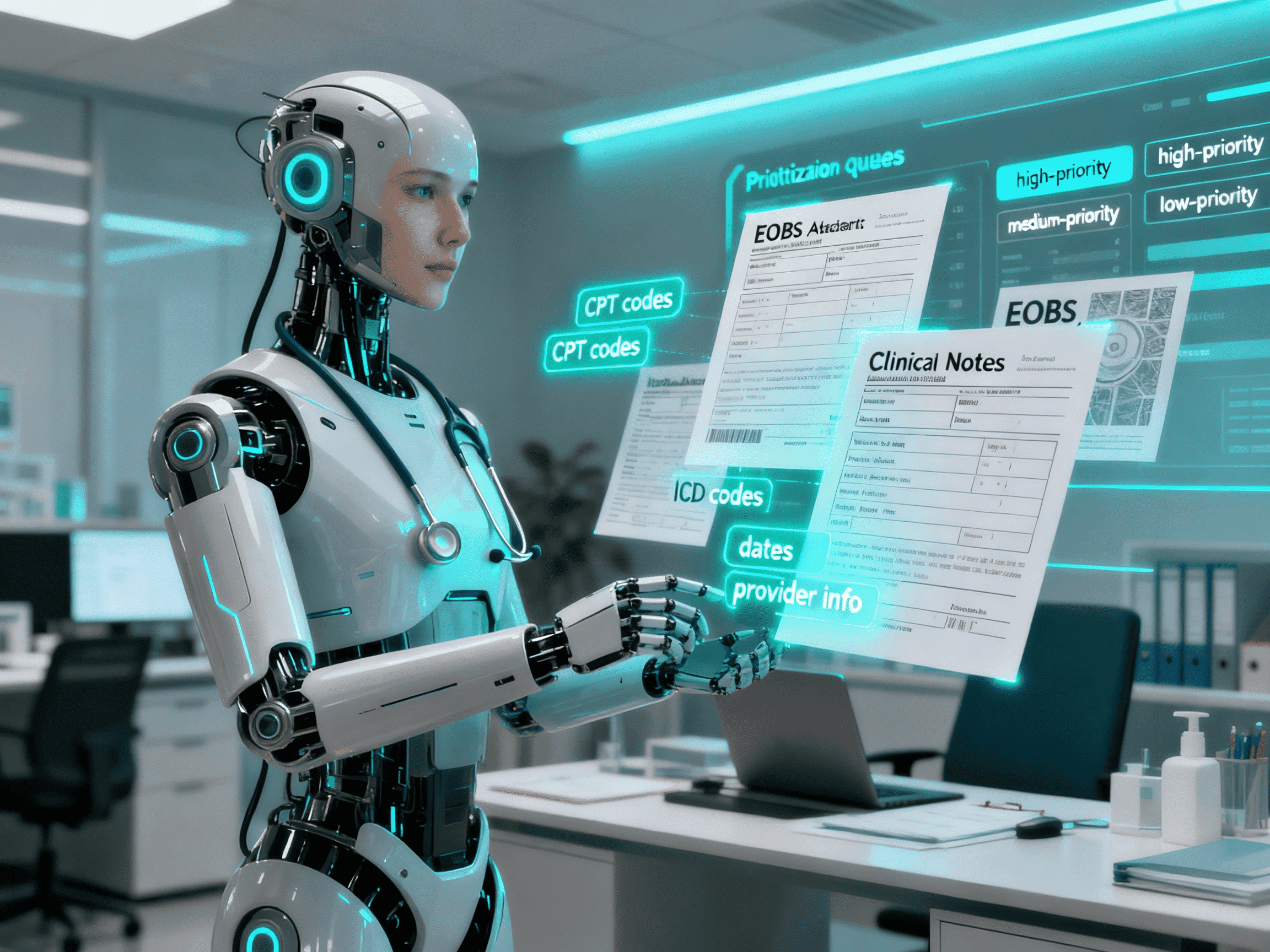
Manual extraction of clinical and billing data from attachments slows claim processing, causes high denial rates, and increases staff workload. Faster, auditable first-pass decisions are needed.
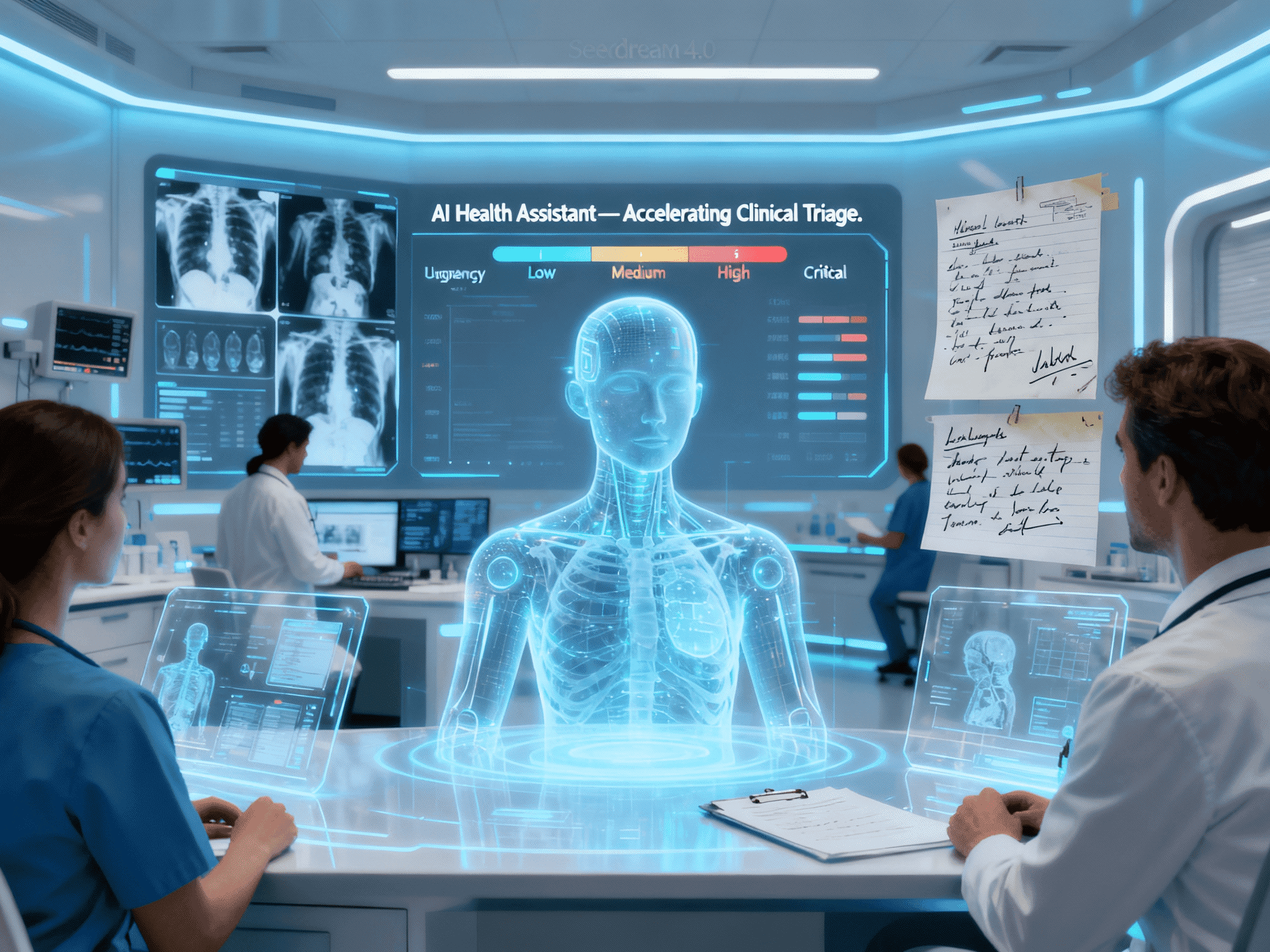
Solution
Lina ingests claims, runs OCR and clinical/billing extraction, validates entries, scores for denial risk, generates appeal text, and produces prioritized queues, enabling faster first-pass resolution.
Result
Reduced claim processing time, fewer manual hours per claim, lower denial and appeal rates, and improved cash flow. Industry benchmarks: 40–75% faster processing, 30–50% shorter escalations.
Use Cases
Lina-Egyptian-Medical-Chatbot streamlines repetitive, error-prone health insurance claims processes. It ingests claims and attachments (clinical notes, EOBs, imaging reports), extracts structured data (CPT/ICD codes, dates of service, provider IDs), validates entries against payer rules, and identifies likely denials with recommended corrections and appeal language. The agent generates prioritized worklists for adjudicators, standardized claim packets (CSV/JSON/PDF), and integrates with storage and ticketing systems to accelerate workflow. Designed for payers, hospital billing teams, and revenue-cycle managers, Lina improves first-pass accuracy, reduces manual rework, and enables human reviewers to focus on clinical exceptions and high-value decisions. ([Amazon Web Services, Inc.][1])
Integrations
Connect to your existing tools seamlessly
Technology Stack
Automation
Automation
Infrastructure
Implementation Timeline
Discovery & Sample Dataset Ingestion
1 weekCollect representative claims, attachments, and denial examples. Define KPIs, data access protocols, and quality requirements to ensure accurate pilot evaluation.
OCR & Extraction Mapping Setup
1 weekConfigure OCR pipelines (e.g., Amazon Textract or Tesseract), create extraction templates, and map clinical and billing fields (CPT/ICD codes, dates, provider IDs) for automated processing.
Risk Rules & Checklist Configuration
1 weekBuild denial-risk scoring rules and mapping to payer policies. Configure automated checks and appeal suggestion templates to reduce human errors and streamline adjudication.
Pilot Batch Review & Tuning
1-2 weeksRun pilot batches, measure extraction accuracy and false positives, and fine-tune models. Collect adjudicator feedback to optimize AI performance and workflow efficiency.
Integration with Storage, Notifications & Reporting
1 weekConnect the agent to claim systems, document storage (AWS S3, SharePoint, Google Drive), communication channels (Slack, MS Teams), and analytics dashboards (Power BI, Tableau) for end-to-end workflow visibility.
Handover, Training & Production Rollout
1 weekProvide documentation, training sessions, and onboarding support. Monitor production performance, refine configurations, and ensure a smooth transition to live operations.
Support Included
30-day tuning included; optional SLA with 24/7 support, model retraining, and compliance audits